What is
Articular cartilage?
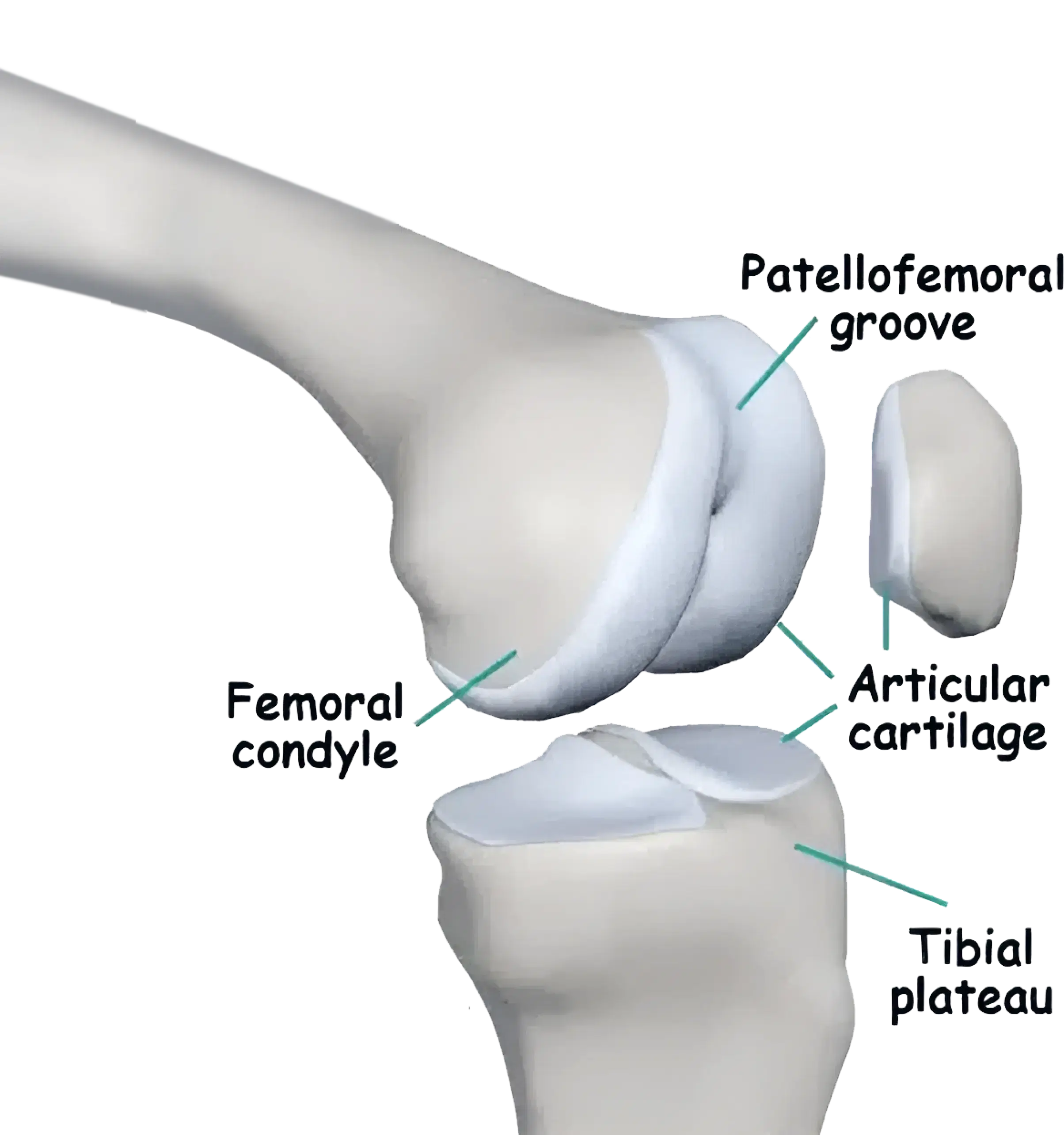
Articular cartilage, a smooth tissue lining the joint surfaces, consists of water, protein, and collagen. Its role is to provide a low friction surface, allowing the joint to bear weight and move smoothly during activity. In essence, it acts as a shock absorber.
The end of the femur (thigh bone)
The top surface of the tibia (shin bone)
The back surface of the patella (kneecap)
How is articular cartilage injured?
Articular cartilage can be injured by
A traumatic injury
Progressive degeneration (covered in knee arthritis)
This section will cover traumatic cartilage injuries
Is articular cartilage
damage a normal part of aging?
Articular cartilage damage is not simply a matter of “wear and tear” or a normal part of aging.
Although the incidence of cartilage damage is increased with increasing age, there are many elderly patients with normal articular surfaces in their knees. In addition to this, there are lots of ultra-endurance athletes who run or hundreds of kilometres yet do not have damaged cartilage.
On the contrary, some have a thicker cartilage layer than is usual, indicating that it is just simply “wear and tear”.

What types of injuries
cause damage to articular cartilage?
Injuries that can be associated with articular damage include
Direct blows to the joint

Dislocation of a joint
A ruptured knee ligament


What
symptoms may I have?
Sudden damage to articular cartilage is usuallly a traumatic event and associated with pain and significant swelling
It is often indistinguishable from other major injuries to the knee such as ligament injury, a dislocation or a fracture. More commonly though, the patient may notice the insidious onset of pain. The pain may be worsened by activity, be associated with swelling, and tends to settle with rest
The pain usually fluctuates in severity and generally deteriorates with time.
How is it diagnosed?
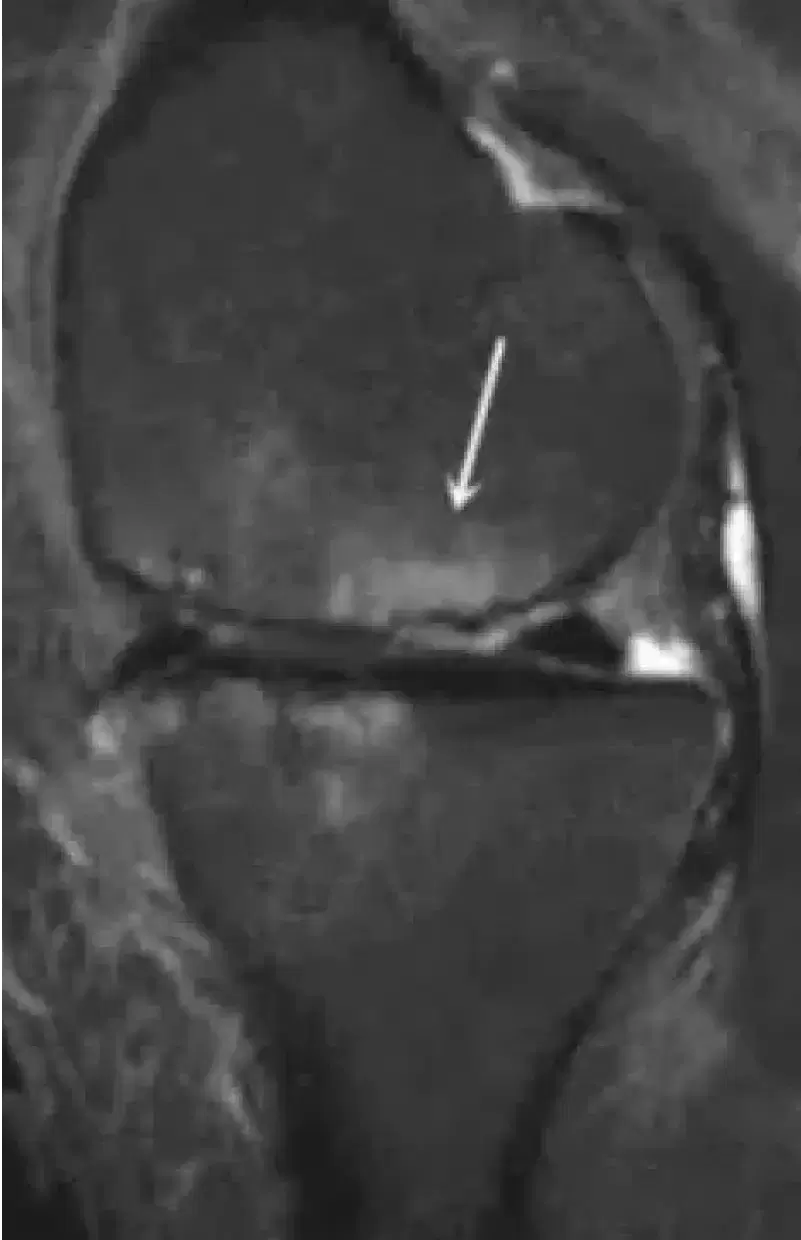
X-rays are used to visualise bone and for this reason articular cartilage cannot be seen with x-rays unless the damage is severe/advanced. The diagnosis is usually made using MRI scans where the cartilage damage can be visualised.
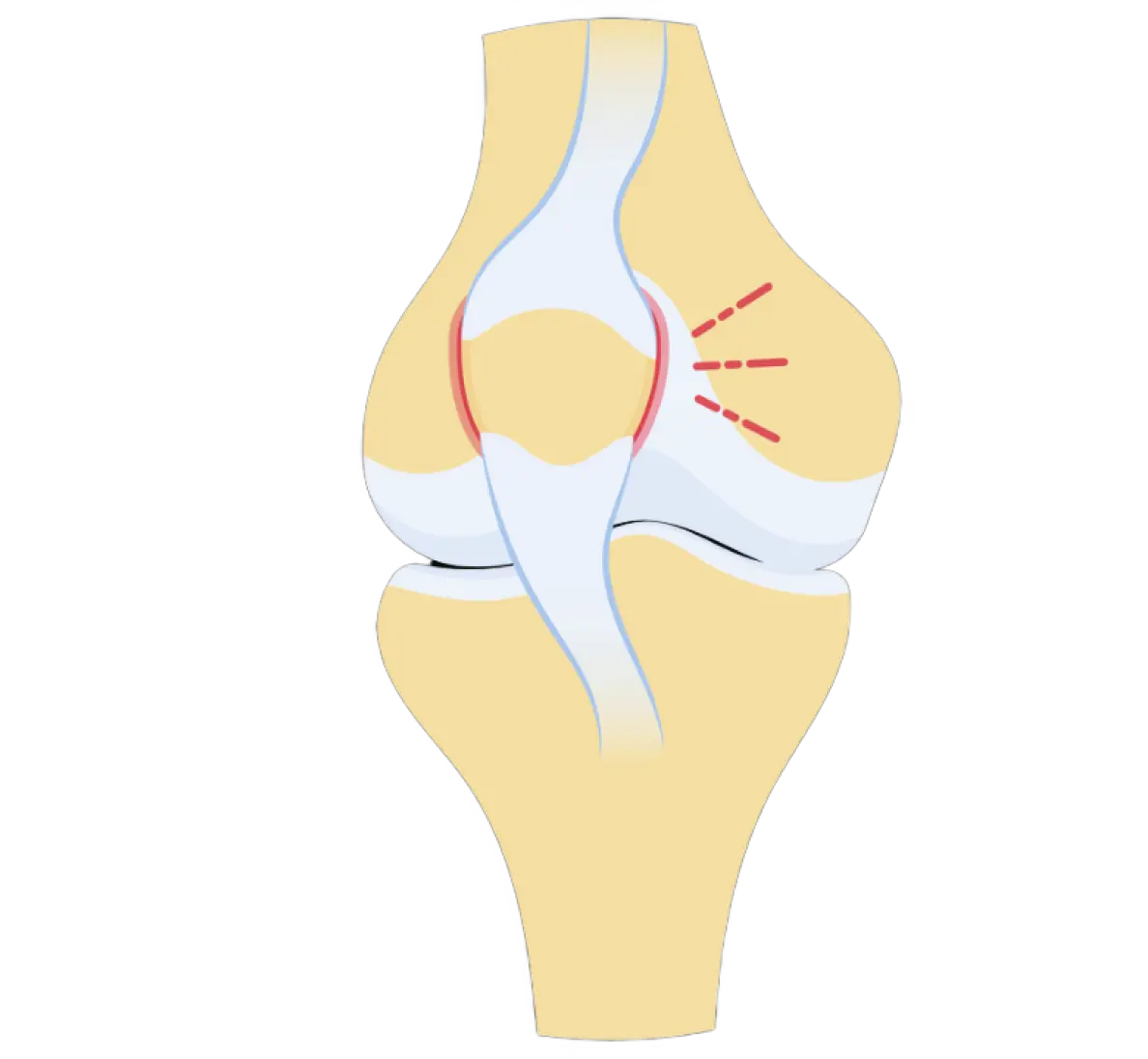
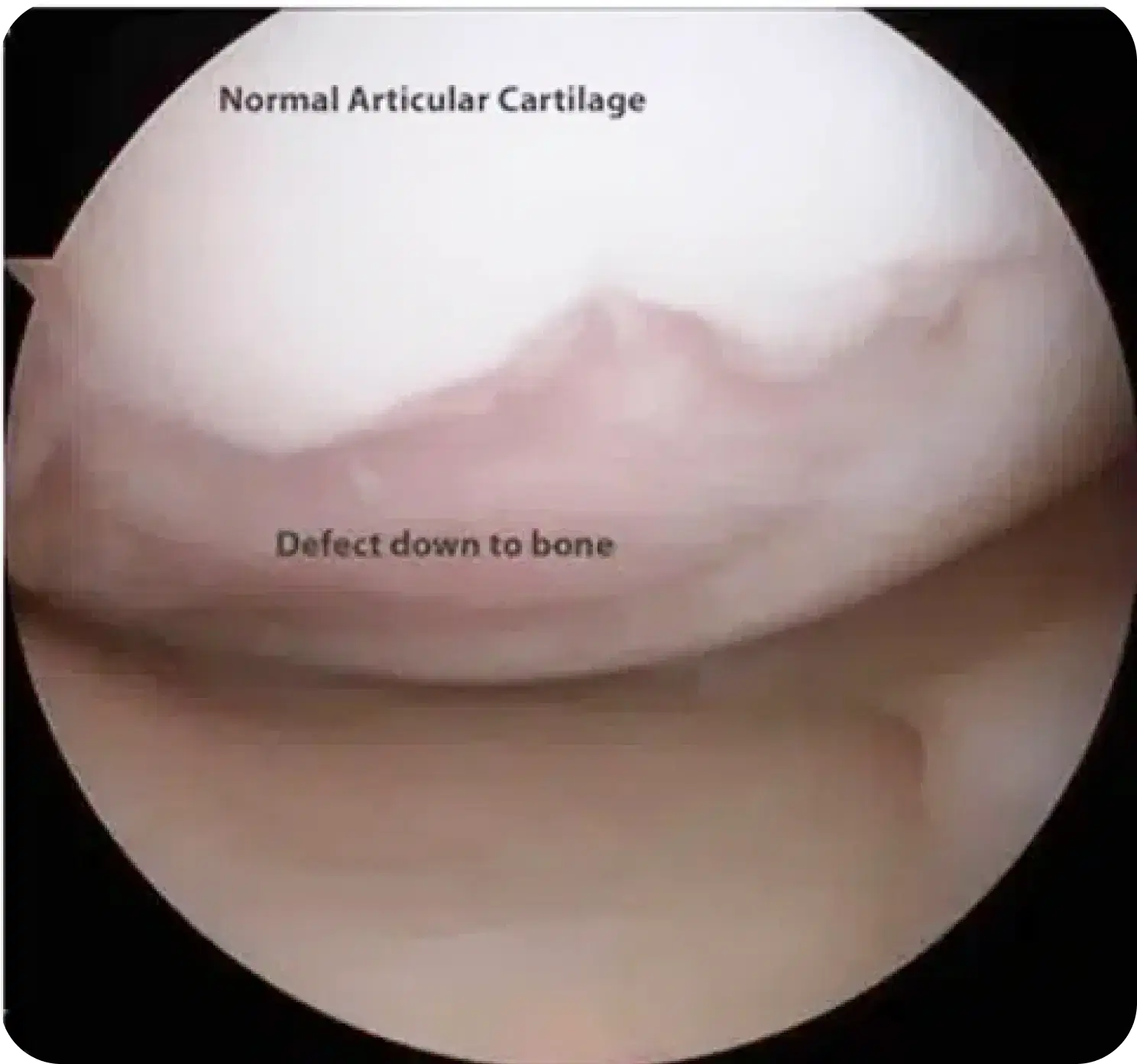
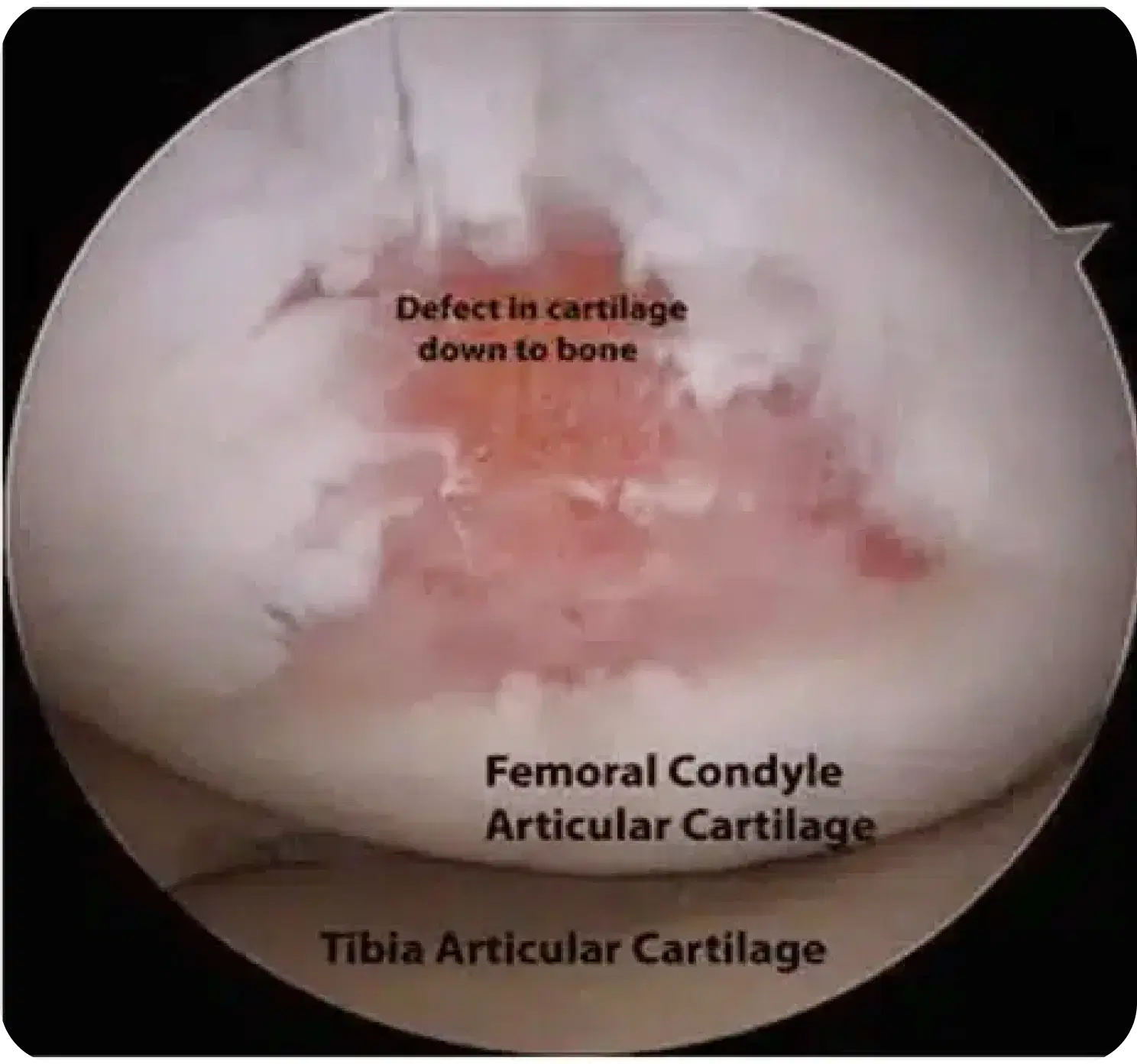
Cartilage damage has a spectrum of severity
On the mild end of the spectrum this can be merely softening of the cartilage. As the disease process worsens, the cartilage can develop areas of thinning, cracks or flaps of cartilage forming.
At the severe end of the spectrum there is complete loss of the cartilage surface and exposed bone is visible.
Articular cartilage cannot be visualised with x-rays. The diagnosis is made using MRI scans where the cartilage damage can be visualised.
An MRI scan allows to determine size and location, as well as whether is possible to repair the damage.
Examples of areas of articular cartilage damage (arrows)
A

B
C

Will I need to have surgery?
The need for surgery depends of
Where the damage is?
The size of the damaged cartilage?
How stable the damage is?
The patient’s age?

What surgical options
are there?
Surgical options include:
Removing the damaged piece of cartilage
And cleaning up where it came from (debridement)
And drilling the bone where the cartilage came from (microfracture)
Repairing the piece of cartilage with screws or darts
Cartilage transplant procedures (MACI or OATS)
Limb realignment (osteotomy) to unload the area of the knee where the cartilage damage occurred

Who is
Suitable for Cartilage Surgery
Most candidates for cartilage repair are young adults with a single injury, or lesion. The size and location of the lesion and the status of other knee structure will help determine wheter surgery is possible for you
Older patients or those with multiple joint lesions are less likely to benefit from the surgery, as it aligns more with osteoarthritis.
To improve the chance of sucess additional procedures could be recommended, these could include
Knee realignment (osteotomy)
Ligament reconstructions (to stabilise the knee)
Book a consultation
today
9:00 am - 4:30 pm
